How Does Hipaa Affect Family and Community Health?
HIPAA: Impacts and Deportment by States
12/30/2014; material added May 2018
The Wellness Insurance Portability and Accountability Act of 1996, known as HIPAA, continues to accept a wide impact on state wellness policy, equally well every bit on virtually all health providers, insurers and health consumers. Listed below are brief updates and resource of potential interest to state legislatures.
-
HIPAA and Protecting Health Data in the 21st Century -
"Inorthward March 2018, the Trump administration appear a new initiative, MyHealthEData , to give patients greater access to their electronic health record and insurance claims information.ane The Centers for Medicare & Medicaid Services will connect Medicare beneficiaries with their claims data and increase pressure on health plans and health intendance organizations to use systems that allow patients to access and send their health data where they like. MyHealthEData is part of a broader move to make greater utilise of patient information to improve care and health. -Article by JAMA, May 24, 2018 - HIPAA at 20: A Bipartisan Accomplishment - Excerpt from release past: U.S. Department of Health and Human Services (HHS) andDepartment of Labor andDepartment of Treasury - August xix, 2016. |
"On Baronial 21, 1996, our nation committed to transforming wellness intendance coverage with the enactment of celebrated, bipartisan legislation called the Wellness Insurance Portability and Accountability Human action of 1996, or HIPAA for brusk.
Many are familiar with HIPAA as a medical privacy and security law. But it is that and and then much more than. A fundamental component of HIPAA's initial purpose was to let people to transfer and keep wellness insurance after they change or lose a job. This was first made possible in 1985 past passage of health insurance continuation provisions in the Consolidated Motorcoach Upkeep Reconciliation Act (COBRA). HIPAA and so congenital upon these gains, and most recently, the Affordable Care Act (ACA) amended and expanded many of the original HIPAA consumer protections. [Read the full statement] - TheAffordable Care Act required HHS, in consultation with the Health Data Technology (HIT) Policy Committee and the HIT Standards Committee, to develop interoperable and secure standards and protocols that facilitate electronic enrollment of individuals in federal and state health and human services programs. To view the recommendations made by the Committees click here. A number of the recommendations address HIPAA related issues.
- JULY 2018 INPUT from JAMA
-
How HIPAA Harms Care, and How to Finish It- Donald 1000. Berwick, Md, MPP; Martha East. Gaines, JD, LLM. JAMA . 2018;320(3):229 doi:10.1001/jama.2018.8829
-
HIPAA and Protecting Health Information in the 21st Century- I. Glenn Cohen, JD; Michelle 1000. Mello, JD, PhD. JAMA . 2018;320(3):231 doi:10.1001/jama.2018.5630
-
Health Data and Privacy in the Digital Era- Lawrence O. Gostin, JD; Sam F. Halabi, JD, MPhil; Kumanan Wilson, MD, MSc.
-
-
HHS rule protects patient privacy, redefines health information distribution (2013-2016).
HHS seeks to modify stringent privacy rules on substance-abuse treatment records - Feb. iv, 2016.HHS proposes to revise a stringent federal rule governing the privacy of medical records of drug, alcohol abuse and many behavioral health patients. Read More
Privacy Rules Apply to ACA.On January 17, 2013 U.S. Health and Human Services' Office for Civil Rights released its terminal regulations expanding privacy rights for patients and others. These new rules trigger major changes in medical tape privacy measures required of wellness providers by ii federal laws, the Health Insurance Portability and Accountability Act (HIPAA, enacted in 1996) and the Wellness Information Applied science for Economic and Clinical Health Act. (HITECH, enacted in 2009),
Although non written specifically for the ACA, these rules utilize to virtually all people insured or treated, including those newly covered through exchanges, private employer coverage, and Medicaid expansions . "This final charabanc rule marks the most sweeping changes to the HIPAA Privacy and Security Rules since they were first implemented," said HHS Office for Civil Rights Manager Leon Rodriguez. The rules expand privacy measures to apply to additional groups that have admission to patient information "regardless of whether the information is existence held by a health plan, a health care provider, or one of their business assembly."
The concluding regulations, published Jan 25, 2013, spell out the new HIPAA compliance obligations of business organization associates and — for the first time — directly regulate thousands of "subcontractors." Among many things, the dominion also prohibits health plans from using genetic information for underwriting (every bit called for under the Genetic Information Nondiscrimination Human activity, GINA, enacted in 2008) and adds new privacy restrictions on wellness-related businesses engaged in marketing and fundraising. I of the highlights of the rulemaking is the creation of a clearer process to determine when patients must be notified of a "breach" in their medical tape privacy.
The HHS issued a summary release which included this data:
The final double-decker dominion greatly enhances a patient's privacy protections, provides individuals new rights to their health data, and strengthens the government's power to enforce the law.
"Much has changed in health care since HIPAA was enacted over fifteen years ago," said HHS Secretarial assistant Kathleen Sebelius. "The new rule will help protect patient privacy and safeguard patients' wellness information in an always expanding digital age."
The changes in the terminal rulemaking provide the public with increased protection and control of personal wellness data. The HIPAA Privacy and Security Rules have focused on wellness intendance providers, health plans and other entities that process health insurance claims. The changes announced today expand many of the requirements to business associates of these entities that receive protected health information, such as contractors and subcontractors. Some of the largest breaches reported to HHS have involved business concern associates. Penalties are increased for noncompliance based on the level of negligence with a maximum penalization of $1.5 million per violation. The changes as well strengthen the Health Data Technology for Economical and Clinical Health (HITECH) Alienation Notification requirements by clarifying when breaches of unsecured hea lth data must exist reported to HHS.
Individual rights are expanded in important ways. Patients can ask for a copy of their electronic medical record in an electronic form. When individuals pay by cash they can instruct their provider non to share information about their treatment with their health programme. The final autobus dominion sets new limits on how information is used and disclosed for marketing and fundraising purposes and prohibits the sale of an individuals' health information without their permission.
"This final jitney dominion marks the most sweeping changes to the HIPAA Privacy and Security Rules since they were get-go implemented," said HHS Function for Civil Rights Director Leon Rodriguez. "These changes not only greatly heighten a patient's privacy rights and protections, merely besides strengthen the ability of my office to vigorously enforce the HIPAA privacy and security protections, regardless of whether the data is being held by a health plan, a health intendance provider, or one of their business associates."
The concluding rule also reduces burden by streamlining individuals' ability to authorize the employ of their health information for research purposes. The rule makes it easier for parents and others to give permission to share proof of a kid'due south immunization with a schoolhouse and gives covered entities and business organization associates up to one twelvemonth subsequently the 180-day compliance date to alter contracts to comply with the rule.
The last omnibus dominion is based on statutory changes under the HITECH Human activity, enacted as part of the American Recovery and Reinvestment Human activity of 2009, and the Genetic Information Nondiscrimination Act of 2008 (GINA) which clarifies that genetic information is protected under the HIPAA Privacy Dominion and prohibits almost wellness plans from using or disclosing genetic data for underwriting purposes.
- The final omnibus rule of 2013 may be viewed in the Federal Register pastpolicymakers and the public, at OCR-PRIVACY-Listing
-
Infographic: HIPAA Privacy and Security Rules Cheat Sheet - This infographic [PDF download] looks at how information breaches occur, how to prevent a breach and the risks surrounding mobile devices. The infographic also provides a HIPAA checklist based on the Department of Health and Human Services' recently released guide to the Privacy and Security of Electronic Wellness Information. a commercial product aimed at providers, available at no charge from Healthcare Intelligence Network - August 2015
Federal Guidance: Court Rulings Extend HIPAA Provisions to All Married Couples
Since the U.Southward. Supreme Court ruled in June 2013 that the portion of the federal police defining "matrimony" every bit a legal matrimony betwixt a human being and a woman was unconstitutional, federal agencies accept been reviewing their regulations to see which may need to exist altered to grant sure rights to married gay couples. In September 2014 , the HHS Role for Ceremonious Rights (OCR) issued guidance clarifying that, as a result of Windsor v. United States , the definition of "matrimony," "family" and "dependent" in the privacy rule was expanded to include same-sex couples who are legally married.
Given the 2013 ruling these terms now "apply to all individuals who are legally married, whether or non they alive or receive services in a jurisdiction that recognizes their marriage," co-ordinate to the OCR guidance, which was published on Sept. 17, 2014. [Read total article]
STATE- BASED Resource
- HIPAA Basics: Medical Privacy in the Electronic Age- Privacy Rights Clearinghouse, revised February 2013.
- FAQ on medical privacy
- State Laws on Access to Medical Records- Georgetown Academy Centre on Medical Record Rights and Privacy. Includes 50 country-specific reports. [link accessed iv/2013]
-
Sharing of Health Information - Federal Laws Governing Privacy of. Medical Information , NCSL slide presentation, R. Morgan and S. Silverman. 2009
HHS Electronic Wellness Record (EHR) Regulations
In 2010, U.S. Department of Health and Human Services Secretary Kathleen Sebelius appear terminal rules to help ameliorate Americans' wellness, increase safe and reduce health care costs through expanded apply of electronic health records (EHR). "Health care is finally making the engineering science advances that other sectors of our economy began to undertake years ago," Dr. Blumenthal said. "These changes volition exist challenging for clinicians and hospitals, simply the time has come to act. Adoption and meaningful use of EHRs volition assist providers deliver better and more effective intendance, and the benefits for patients and providers akin will abound rapidly over fourth dimension."
- Modifications to Meaningful Use for 2015 through 2017: Realigning the EHR Incentive Programs to back up wellness information exchange and quality improvement. On April 10, 2015, the Centers for Medicare & Medicaid Services issued a new proposed rule for the Medicare and Medicaid Electronic Health Record (EHR) Incentive Programs to marshal Stage one and Stage two objectives and measures with the long-term proposals for Stage three, to build progress toward plan milestones, to reduce complexity, and to simplify providers' reporting. These modifications would let providers to focus more closely on the advanced utilise of certified EHR engineering science to back up health information exchange and quality improvement.
Better Care, Smarter Spending and Healthier People. The proposed rule is just 1 part of a larger endeavour across HHS to deliver better care, spend wellness dollars more than wisely, and have healthier people and communities by working in three cadre areas: improving the fashion providers are paid, improving the manner intendance is delivered, and improving the style information is shared to support transparency for consumers, health care providers, and researchers and to strengthen decision-making.
NOTE: NCSL provides links to other Web sites from time to fourth dimension for information purposes only. Providing these links does non necessarily betoken NCSL'south back up or endorsement of the site.
Health Information technology (Includes archive materials)
- An NCSL report describes and provides links to specific land legislation on Hit and public reporting: www.ncsl.org/programs/health/Transparency.htm. - Updated 2015.
-
HIPAA functions expanded by HITECH Act- Amidst other HIPAA changes fabricated in the new law (all of which should be of business concern to health care providers, health care payors, health intendance clearinghouses- "covered entities" or CEs- and their "business assembly"- vendors who touch electronic protected health information or ePHI), there is a provision that permits land attorneys general to file HIPAA enforcement deportment on behalf of the people of their land, in order to protect their interests, and to seek injunctive relief and/or money damages. See Sec. 13410(eastward) of ARRA (p. 160 of HR i PDF). A web web log posting titled "HIPAA enforcement by land attorneys general: The shape of things to come" provides details on a CT case. 1/fifteen/2010.
-
Profiles of Progress 4: State Health IT Initiatives - published by NASCIO, July 2010.
-
Office of the National Coordinator for Health It, U.s. Section of Wellness and Human Services
-
"fifty Lilliputian Labs: States are performance as proving grounds for healthcare information technology initiatives" - Healthcare Infomatics, 10/08.
-
FTC Sets Dominion Requiring Public Notification of PHR Breaches. In mid-Baronial 2009, the Federal Trade Commission issued a concluding rule requiring personal health record providers to alert consumers near data security breaches. The rule also requires organizations to notify the media if the security breach involves more than 500 people. FTC's regulations will utilize to Google Wellness, Microsoft HealthVault and others. Authorities Health IT, Wellness Information Management. eight/20/09.
- "Profiles in Progress: State Health It Initiatives," by the National Clan of State CIOs, a compendium highlighting health IT initiatives in all 50 states and D.C. Released xi/fifteen/06 [54 pages, PDF]
-
Wellness Information technology: Efforts Proceed but Comprehensive Privacy Approach Needed for National Strategy- Study by the Government Accountability Office identifies challenges that the Department of Wellness and Man Services faces in trying to protect electronic patient data. Yet, HHS says that information technology already has adopted a privacy approach. six/nineteen/07. [23 pages, PDF]
-
CMS Gears Up for South Carolina Test of Personal Health Records- The Centers for Medicare and Medicaid Services projection will offer personal health records to 100,000 participants in Southward Carolina's Medicare fee-for-service program and volition include a campaign to encourage use of the PHRs. The results of the South Carolina project will be compared with the results of earlier PHR initiatives. Government Health IT , one/21/08.
-
HIPAA-covered entities such as providers completing electronic transactions, healthcare clearinghouses and big wellness plans must employ simply the National Provider Identifier (NPI) to identify covered healthcare providers in standard transactions, effective May 23, 2007. All such organizations need to ensure they are prepared for the (NPI) May 2007 borderline.
-
2006 Minnesota e-Wellness Initiative Progress Report to the Minnesota Legislature [23 pages, PDF] and Minnesota e-Health Reports and Recommendations.
-
eHealth Initiative - an association with data on commercial and governmental projects. Updated regularly.
-
Report: Three-quarters of states are developing HIEs. Published on April 22, 2008 (c) Govt. Wellness IT: Iii-quarters of states have begun developing some kind of health data substitution, co-ordinate to a report released today by the State-Level HIE Consensus Project. The project's director, Lynn Dierker of the American Health Information Management Association, told a Health and Human Services Department advisory console that the need for health care reform generally falls backside the creation of state-level HIE organizations, forth with the need to keep patients' data private and secure. Some HIEs have advanced to the betoken where they are nearly ready to begin exchanging information, Dierker told the American Health Information Community. "We experience like we are labs" for the exchange of patients' wellness information, she said.
The HIEs are public/private partnerships and seldom part of state governments, she said. They usually include stakeholders from many interest groups, and they serve the public involvement, operate toll-finer and protect the privacy of patients whose records move through the network. Although governance responsibilities are the almost common role of state-level HIEs, Dierker said, the organizations are often responsible for the technical operations, too. A new national organization called the State-Level HIE Leadership Forum is emerging to share insights and lessons learned, she said. Information technology will hold its first coming together in May in Dallas.
Also, state-level HIEs want to participate in AHIC'due south successor system, which is being created as a public/private partnership outside HHS, Dierker said. Synergy is needed between national and land-level health it programs and other wellness reform initiatives such as quality-of-intendance measurement and pay-for-operation incentives. Amid other activities in the coming year, the project will determine whether it is desirable to ascribe HIEs that meet certain criteria and how to sustain organizations after a kickoff-upward period. In addition, the relationship of land-level HIEs to the planned Nationwide Health Information Network remains undefined, the report states. Those who pay for health care should exist more involved in HIE development, the report states. "At a national level, the roles for Medicaid and Medicare in helping to build and sustain HIE chapters must be clarified and strengthened," it states. "The active engagement of health plans in strategies to support state-level HIE remains an important priority." The Office of the National Coordinator for Health IT supports the Country-Level HIE Consensus Project. -
Serious patient errors at California hospitals disclosed in state filings. Most 100 Californians a month are beingness harmed in adverse events considered preventable. A lawmaker proposes banning reimbursements to hospitals for some types of injuries. Maine, Massachusetts, Pennsylvania and New York have restricted payments for avoidable medical errors. Hospital associations in Minnesota, Washington and Vermont take pledged never to bill patients for the costs of botched care, co-ordinate to the National Conference of Land Legislatures. LA Times, 6/30/08.
-
Physician Use of Electronic Prescribing and Barriers to Adoption
- Despite the benefits of electronic prescribing, adoption is even so minor. Current surveys estimate that between 5% and xviii% of physicians and other clinicians are using electronic prescribing.
- Fundamental barriers to clinician adoption include startup cost, lack of specific reimbursement, and fright of reduced efficiency in the practice.
- The implementation of the prescribing system must fit into the business menstruation and raise noesis, rather than be viewed as "extra work." Electronic prescriptions need to be seen, in many ways, as an extension of a written prescription, for adoption to occur. The benefits to all parties – pharmacist, clinician and patient – should be the ultimate goal in the adoption of electronic prescribing.
Medical Tape Privacy
Nigh xiii years agone, equally of April 14, 2003 "health plans, hospitals, doctors and other health care providers effectually the country must comply with new federal privacy regulations," according to Secretary Tommy Thompson of the Section of Health and Man Services (HHS). Billions of dollars are being spent to bring public and private sector records into compliance. The following is the department's description,which stated in Apr, 2003: "These new federal health privacy regulations set a national floor of privacy protections that will reassure patients that their medical records are kept confidential. The rules will help to ensure advisable privacy safeguards are in place as we harness data technologies to amend the quality of care provided to patients. Consumers will do good from these new limits on the fashion their personal medical records may exist used or disclosed past those entrusted with this sensitive data."
The new protections give patients greater access to their own medical records and more than command over how their personal information is used past their wellness plans and health care providers. Consumers will get a find explaining how their health plans, doctors, pharmacies and other health care providers apply, disclose and protect their personal data. In improver, consumers will have the ability to run across and copy their wellness records and to request corrections of whatever errors included in their records. Consumers may file complaints well-nigh privacy problems with their wellness plans or providers or with our Part for Civil Rights."
Privacy Online Resources:
- HIPAA Nuts: Medical Privacy in the Electronic Age- Privacy Rights Clearinghouse, revised February 2013.
- FAQ on medical privacy
- Country Laws on Admission to Medical Records- Georgetown Academy Center on Medical Record Rights and Privacy. Includes 50 country-specific reports. [link accessed 4/2013]
- Texas Ambitious New Patient Privacy Police force Could Hit Covered Entities Nationwide. A new Texas police governing the privacy and security of protected health information, perchance the broadest and among the toughest of such laws in the nation, went into event on Sept. one. The Texas Medical Privacy Act, signed into police force June 17, 2011, by Gov. Rick Perry (R), not only increases requirements beyond those in HIPAA for organizations that are already covered entities (CEs), but greatly expands the number and blazon of Texas-based CEs required to comply with the privacy standards in HIPAA and adds a bunch of its own requirements. Information technology contains split mandates for alienation notification of electronic PHI and penalties for violations. Read Full Story [excerpt from Report on Patient Privacy , 9/1/2012]
- Federal Trade Commission Issues Proposed PHR Alienation Dominion - In compliance with the American Recovery and Reinvestment Act, the Federal Trade Committee has issued a proposed dominion that would require personal health record vendors and related groups to notify customers if their identifiable health data is breached, Health Information Direction reports. FTC is seeking public annotate on the proposed rule through June 1. ARRA requires HHS and FTC to publish a written report on potential privacy, security and breach notification requirements for PHR vendors and related entities by Feb 2010. In the concurrently, the law requires FTC to outcome an interim concluding rule by August.-Health Data Management, Modern Healthcare. four/17/09.
-
"Privacy Upshot Complicates Push to Link Medical Data" - article by New York Times, ane/17/09.
-
"New health-intendance privacy laws heighten need for HIPAA compliance in California." Gov. Schwarzenegger signs 2 data privacy bills that use the federal HIPAA law every bit a baseline. ComputerWorld, 10/7/08.
-
"PERSONAL Health DATA ON THE Internet: STATES ADDRESS PRIVACY CONCERNS" - NCSL's State Health Notes, June nine, 2008.
-
Warnings Over Privacy of U.Due south. Health Network - New York Times, 2/18/2007.
-
"Personal Health Records: The People's Choice?"- National Health Policy Forum, 11/30/06.
-
Wellness Data TECHNOLOGY: Efforts Go on only Comprehensive Privacy Approach Needed for National Strategy- Report by the Government Accountability Role identifies challenges that the Department of Health and Human Services faces in trying to protect electronic patient data. However, HHS says that information technology already has adopted a privacy approach. vi/19/07. [23 pages, PDF].
-
Balancing Patient Privacy with the Need to Know Obtaining a patient's health history is vital to ensuring proper treatment, all the same disclosing data about mental wellness or substance abuse can result in social stigma, job loss, or even criminal prosecution. A new result brief considers how best to balance privacy and disclosure in an historic period when sharing data has never been easier. CA Healthcare Foundation cursory, 3/08.
-
Medical Privacy - National Standards to Protect the Privacy of Personal Wellness Information- detailed explanations by the HHS Office for Civil Rights.
Archived Resources:
Electronic Transactions Requirements
Federal regulations required compliance with new HIPAA national standards for electronic wellness care transactions, code sets and national identifiers for providers, health plans, and employers, as of an October 2003 deadline. The federal Administrative Simplification Compliance Act (ASCA) required all claims sent to the Medicare Program be submitted electronically starting October 2003. (This is split up from medical privacy requirements, below.)
- News particular: Meaningful-use deadline pushed back one yr.
HIPAA Administrative Simplification
HIPAA Health and Nondiscrimination
DOL Bug CHECKLIST FOR Health PROGRAMS.
Wellness programs must be carefully reviewed to assure that they fit within a diverseness of legal boundaries. Most important for 2008 and across are the nondiscrimination rules under HIPAA. The Department of Labor (DOL) has issued helpful guidance in Field Help Bulletin 2008-02 (FAB 2008-02), including a useful checklist. This guidance can be reviewed past any policymaker or program sponsor implementing a wellness program or considering one. ["CheckUp" by Sibson, 3/ten/08)
Health promotion or disease prevention programs offered by a group health plan must comply with the Department of Labor's final wellness program regulations, published every bit 29 CFR 2590.702. 29 CFR 2590.702. The final regulations include guidance on the implementation of wellness programs.
HIPAA's nondiscrimination provisions by and large prohibit a grouping health plan or group health insurance issuer from denying an private eligibility for benefits based on a health factor and from charging an individual a higher premium than a similarly situated individual based on a health factor. Wellness factors include: wellness condition, medical condition (including both concrete and mental illnesses), claims experience, receipt of health care, medical history, genetic data, bear witness of insurability (including conditions arising out of acts of domestic violence), and inability. An exception provides that plans may vary benefits (including price-sharing mechanisms) and premiums or contributions based on whether an private has met the standards of a wellness program that complies with paragraph (f) of the regulations. The regulations apply to grouping wellness plans and group health insurance issuers on the outset twenty-four hour period of the program year beginning on or after July one, 2007.
HIPAA Security Rules for 2005
In a carve up procedure, HHS issued a Final Security Rule requiring health plans, certain health care providers and health data clearinghouses to institute "adequate authoritative, physical, and technical safeguards to prevent unauthorized admission to electronic patient health information." Almost covered entities had until Apr 2005 to comply with the new security standards.
Additional Resources
NCSL is not responsible for the opinions and enquiry data reported on third-party websites.
Wellness Privacy- Center for Democracy and Technology's Web folio, which focuses on health privacy issues. The Center for Democracy and Technology works to proceed the Cyberspace open, innovative and free.
APPENDIX 1 - HIPAA at 20
HIPAA at 20: A Bipartisan Accomplishment
"On August 21, 1996, our nation committed to transforming health care coverage with the enactment of historic, bipartisan legislation called the Wellness Insurance Portability and Accountability Human activity of 1996, or HIPAA for short.
Many are familiar with HIPAA every bit a medical privacy and security constabulary. Merely it is that and so much more. A key component of HIPAA'south initial purpose was to allow people to transfer and go on health insurance after they modify or lose a job. This was get-go fabricated possible in 1985 by passage of health insurance continuation provisions in the Consolidated Motorbus Budget Reconciliation Act (COBRA). HIPAA then congenital upon these gains, and nearly recently, the Affordable Care Act (ACA) amended and expanded many of the original HIPAA consumer protections.
Prior to the passage of HIPAA, many people were afraid to modify jobs out of fright that a preexisting medical condition would forestall them from receiving health insurance coverage. HIPAA addressed this concern through its portability provisions, which lessened the possibility that an individual would lose wellness care coverage for a preexisting condition when irresolute to a new employer's group health plan or when seeking coverage in the individual market. HIPAA also required group health plans to provide special enrollment periods for employees and their dependents who feel a qualifying outcome such as loss of other grouping coverage, birth of a child, or marriage.
HIPAA prohibited group health plans from discriminating based on health status against an employee or a dependent in terms of eligibility or price of coverage. The ACA expanded this provision to certain individual health insurance policies. HIPAA also mandated that all individual and group wellness insurance coverage, including minor employers with 2-50 employees, be guaranteed renewable at the option of the private or employer. The ACA connected this protection for both big and modest employers, and most significantly, to individuals and families purchasing individual market wellness insurance policies.
Twenty years ago, a considerable portion of every health care dollar was spent on administrative overhead in processes that involved numerous paper forms and telephone calls, not-standard electronic commerce, and many delays in communicating information among different locations. This situation created difficulties and costs for health care providers, wellness plans, and consumers.
Under HIPAA, standards were adult to amend the way wellness care data is exchanged electronically. HIPAA simplified and encouraged the electronic transfer of information by requiring the HHS to adopt standards for certain electronic transactions, and now 93.8% of all health care claims transactions today are conducted in standard form. The HIPAA standards accept helped pave the way for the interoperability of health information to enhance the patient and provider experience.
HIPAA likewise enhanced privacy and security protections for consumer health data past establishing requirements for most wellness care providers, health plans and other entities that process health insurance claims, and their business assembly to safeguard information. HIPAA's Privacy Rule gives individuals important rights to their health information, and sets rules for how the information can be accessed, used and disclosed. For example, the HIPAA Privacy Rule gives individuals the correct to a re-create of their health information in the form and format that they request – including an electronic re-create.
The HIPAA Security Dominion requires health intendance organizations to safeguard the electronic wellness data they hold. Among the dominion's requirements, organizations covered past HIPAA must engage in comprehensive risk analyses and risk management to ensure that wellness data is secure. This includes implementing physical, technical, and authoritative security measures sufficient to reduce risks in all concrete locations and on all portable devices to a reasonable and appropriate level. Finally, HIPAA was modified in of import ways, including the requirements that breaches of unsecured wellness information are reported to affected individuals, the Department of Health and Human Services, and in some cases the media. This requirement helps individuals know if something has gone incorrect with the protection of their information and helps keep organizations answerable for privacy and security.
Nosotros have come a long way in xx years, but work is non yet done. Every twenty-four hour period, we are seeing breakthroughs in mobile health, including many more consumer-facing health apps with the patient at the middle of the chat. We are seeing improvements in wellness intendance commitment, with many solutions tied to improvements in health intendance-related systems. Wellness care innovation is increasingly not near individual solutions capturing data at the point of care, but rather how information tin be applied and shared across systems for the adept of the population as a whole. HIPAA has been a blue print for health care reform, paving the way for the futurity by making health care commitment more efficient and expanding coverage to more Americans. Together, we gloat 20 years of this celebrated legislation."
APPENDIX two -- Medical Records - Full general Information
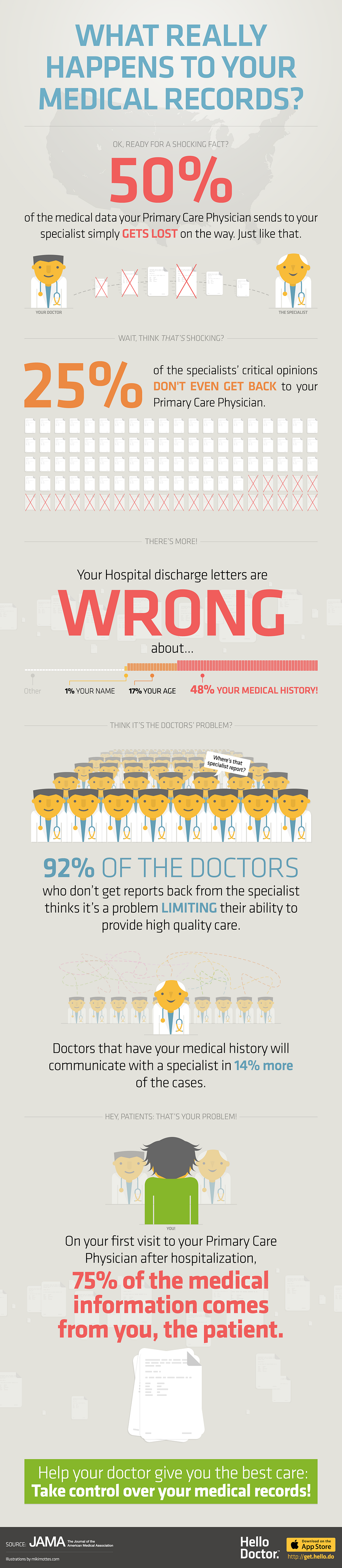
Infographic: What Really Happens to Your Medical Records? Gaps in medical records equal potential gaps in care, they can cause an increment in avoidable readmissions and healthcare costs. Fifty percent of medical information gets lost while being sent from primary care physicians (PCPs) to specialists, according to a new infographic from JAMA andHello Doctor. This infographic includes statistics about imitation information on hospital discharge letters, missed medical data and opinions from specialists to PCPs, effects on quality of care and more. Posted 1/6/2014 (c).
Source: https://www.ncsl.org/research/health/hipaa-a-state-related-overview.aspx
0 Response to "How Does Hipaa Affect Family and Community Health?"
Post a Comment